It is well known that tethered education helps bridge knowledge gaps among healthcare providers and patients alike. This need to bridge these gaps is profound in the realm of triple negative breast cancer (TNBC), where stark racial disparities exist.
The disease disproportionately affects Black and Hispanic women as well as younger women. These disparities may be due to a number of factors, including tumor heterogeneity, population genetics and somatic genomic mutations. In women younger than 40 years of age — who are not eligible for mammography screening — Black women are twice as likely to have an incidence of TNBC than Caucasian women. They tend to experience earlier onset and harbor an aggressive TNBC phenotype. Common breast cancer treatments such as endocrine or hormone therapy are ineffective in this disease, which tends to relapse early after standard chemotherapy.
Outcomes from previous PlatformQ Health breast cancer educational initiatives revealed that significant disparities exist between the care perceptions of healthcare providers and their patients. Many patients and providers are unaware of the increased risk of Black and Hispanic women developing the disease, which may increase disparities. Addressing health literacy about TNBC serves multiple purposes, including:
- To help women better understand risk, obtain appropriate screening and advocate for themselves with their providers
- To increase the suspicion index of providers to drive earlier detection, diagnosis and treatment
TNBC is a historically difficult-to-treat breast cancer subtype. There are expanded treatment options as well as clinical trial opportunities that may benefit many patients. However, providers need to be informed about these to make evidence-based decisions while considering patients’ goals and priorities.
Understanding Tethered Education
To that end, the National Breast Cancer Foundation, Inc., TOUCH — the Black Breast Cancer Alliance and PlatformQ Health partnered to produce a tethered education program. This involved producing separate but aligned educational activities for patients/caregivers and providers that share related themes and goals. The two sessions were designed to close gaps between what an individual sees as their priorities and what their doctor assumes those priorities are. Previous tethered programs in other therapeutic areas have demonstrated an improvement in communication between patients and providers, and the intention was to replicate that model to create a meaningful learning experience that drove improved outcomes.
Tethered Education Timeline
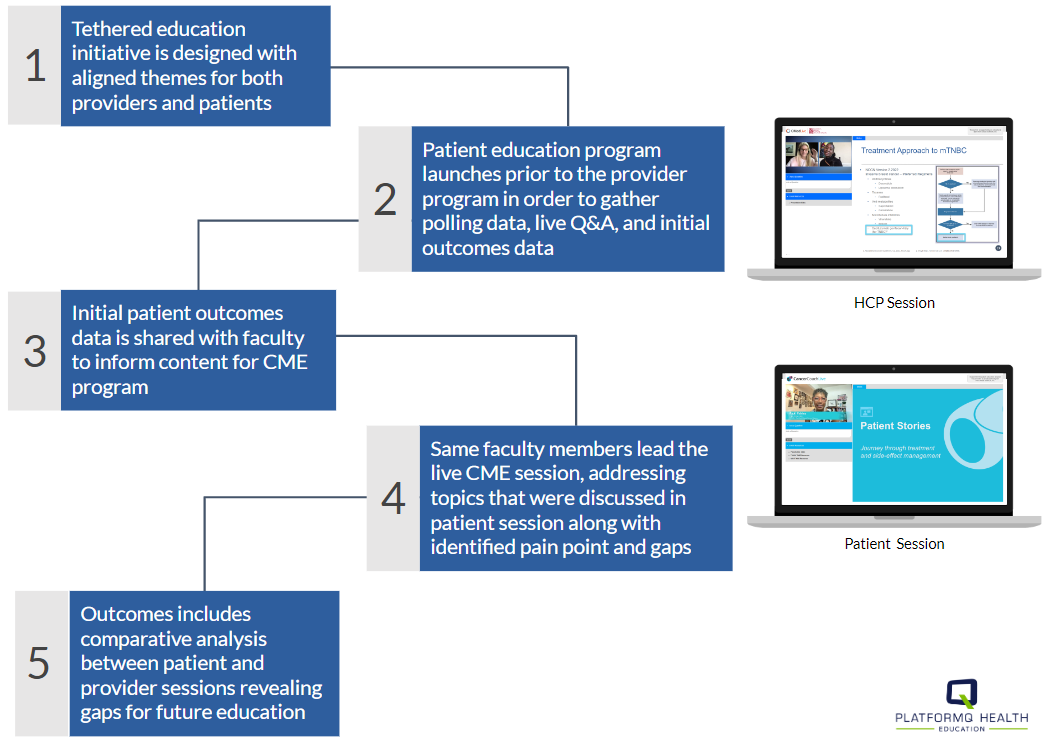
Unlike some tethered programs where the patient and provider sessions occur simultaneously, the TNBC program was designed specifically to gather information during the patient education program that would inform the provider session. The timing of the sessions is also important. As noted in the below workflow, the patient session preceded the provider session, and data from it was used to develop and hone content for the provider session held one month later.
Program Overview
The initiative addressed knowledge gaps among providers related to socioeconomic and racial or ethnic risk factors that lead to worse outcomes for Black and Hispanic women diagnosed with TNBC. Tethered patient and provider activities that met the needs of both audiences served to improve and inform shared dialogue, goal setting and decision-making.
For both the patient and provider sessions, a panel discussion was led by two oncologists as well as a patient advocate from TOUCH. The session incorporated pre-taped patient video vignettes to ensure patient perspectives were included to help frame discussions of case studies and treatment planning in TNBC.
Educational Session for Patients and Caregivers
The patient/caregiver session was far reaching, covering:
- Factors that impact the risk and prognosis of TNBC
- The importance of self-advocacy and shared decision-making
- Approved treatments for locally advanced or metastatic TNBC
- Participation in clinical trials, communication with teams, and finding support and resources
- Reducing the potential of cancer being dismissed by a provider due to misconceptions about TNBC
- Types of tests to determine TNBC
- Side effects of treatment and ongoing supportive care
- A patient vignette addressing the journey through treatment and side-effect management
Knowledge Gaps Among Patients and Caregivers
Twenty-nine thousand seven hundred seventy-four patient and caregiver learners participated in the first session, entitled “Facing TNBC: Self Advocacy and Decision Making.” Pre-test surveys revealed knowledge gaps, including the fact that many women lacked awareness about the risk factors associated with developing TNBC, the disparities that exist in TNBC and available treatment options. These insights helped inform the content for the provider session.
Knowledge Gaps Among Providers
Knowledge gaps identified prior to the session included lack of recognition of racial and ethnic disparities, the role of genetic testing and trial selection, and how to integrate recently approved agents into clinical care. It was also clear that there was room for improvement when it came to sensitivity to each patient’s journey and understanding how to facilitate patient-centered care.
There was also a misalignment between patients and providers on the topic of clinical trial diversity, with providers identifying “patient lack of interest” as a barrier to clinical trials yet 60% of patient participants indicating that, if eligible, they were very likely to participate.
Based on these knowledge gaps, the provider session, entitled “Addressing Disparities in Care and Integrating Antibody Drug Conjugates as Treatment for Patients with TNBC,” focused on:
- Challenges encountered by ethnic minority patients with TNBC
- Solutions to address disparities in care for women of ethnic minorities diagnosed with TNBC
- Recent advances in TNBC pathogenesis and prognosis
- Coordinating referrals to genetic testing and counseling
- Evaluating the mechanisms of action as well as safety and efficacy data for emerging TNBC agents
- Strategies for facilitating patient-centered care through accounts of real-world patient experiences
- Social factors impacting survival of TNBC patients
- Considerations of patient selection for antibody drug conjugate treatment
- Side-effect management, including sharing patient voice to understand patients’ perceptions about side effects
Gauging Initial Session Outcomes
A comprehensive outcomes process was used to capture the impact of the learning sessions on clinical practice, identify remaining gaps and barriers to care, and provide actionable guidance for future education. This included in-depth surveys conducted immediately following as well as two months after each session, with the opportunity to share write-in comments.
For the patient/caregiver session, the average time in session exceeded 27 minutes.
Sixty-six percent of learners reported that the program positively impacted their communication with providers, and 60% reported that they feel more in front of their health-related decisions.
Three hundred eighty-seven healthcare providers participated in the accredited CME program, with a nearly 25-minute average time in session. Fifty-five percent of learners reported the activity had a positive impact on their clinical practice, and 50% reported a positive impact on patient outcomes or experiences. The pre- and post-session questions demonstrated an increase in competencies across learning objectives.
Key Takeaways
Having the right partners was integral to the success of the tethered educational programs. This educational partnership facilitated an assessment of attitudes, perceptions and barriers to care that can further guide how disparities in care for patients with TNBC are addressed. This “tethered” approach was successful in empowering patients and initiating changes in clinical practice for patients with TNBC.
Learn more about applying tethered education to improve outcomes.
Read more from the authors in the article “Advancing the Patient's Role in CME/CE” on the Almanac.
 Tariqa Ackbarali is the senior medical director for oncology at PlatformQ Health. She has been in the CME industry for more than 12 years, primarily focused in the area of oncology/hematology. She earned her Doctor of Philosophy in health sciences from Nova Southeastern University and received both her B.S. majoring in psychology and minoring in biology and her M.S. in clinical psychology from Barry University. Prior to joining the Institute for Medical Education and Research (IMER) in 2009, she completed a practicum and internship at the Children’s Diagnostic and Treatment Center, a medical home setting providing counseling and testing services to children and parents. Dr. Ackbarali served the medical education industry at Rockpointe in 2012 and then PRIME Education in 2017 where she was responsible for oncology/hematology educational program growth, including execution of multiple quality improvement programs. Dr. Ackbarali continues her passion for creating tangible impact through education at PlatformQ Health, where she educates both clinical teams and patients/caregivers.
Tariqa Ackbarali is the senior medical director for oncology at PlatformQ Health. She has been in the CME industry for more than 12 years, primarily focused in the area of oncology/hematology. She earned her Doctor of Philosophy in health sciences from Nova Southeastern University and received both her B.S. majoring in psychology and minoring in biology and her M.S. in clinical psychology from Barry University. Prior to joining the Institute for Medical Education and Research (IMER) in 2009, she completed a practicum and internship at the Children’s Diagnostic and Treatment Center, a medical home setting providing counseling and testing services to children and parents. Dr. Ackbarali served the medical education industry at Rockpointe in 2012 and then PRIME Education in 2017 where she was responsible for oncology/hematology educational program growth, including execution of multiple quality improvement programs. Dr. Ackbarali continues her passion for creating tangible impact through education at PlatformQ Health, where she educates both clinical teams and patients/caregivers.