Alliance Almanac article accompanying the 2023 Excellence in Educational Design Award
Introduction
While the rapidly evolving field of immuno-oncology (I-O) has precipitated unprecedented advancements in cancer treatment, there are significant clinical gaps related to I-O biomarker testing and patient care. One of the consequences of these gaps is that patients who could potentially benefit from targeted I-O therapies do not get the most appropriate testing or treatments they need. For patients to receive the optimum benefit from advances in I-O therapies, the multidisciplinary cancer care team (which includes physicians, laboratory professionals and other healthcare providers) needs education on the implications that I-O biomarkers pose for selecting I-O therapies and assessing patient response to treatment. There are also equity-related issues to address to ensure that patients have access to these life-extending therapies.
Addressing these needs was central to the educational program designed by the American Society for Clinical Pathology (ASCP) and Q Synthesis to lead change in the delivery of I-O biomarker testing and care, aimed at building scientific knowledge around I-O biomarkers and expanding the use of I-O biomarker testing in community healthcare settings. The program accomplished these aims, addressing key gaps in the multidisciplinary team’s ability to keep up with the latest developments in I-O therapies and the implications for biomarker testing, and helping them identify practical ways to overcome barriers that lead to delayed I-O biomarker testing, inefficient testing methods and disparities in testing among different patient groups. This article summarizes the components of the educational program and highlights key outcomes, including improvements in patient care. It demonstrates ASCP’s approach to facilitate implementation of practice changes and highlights the program’s flexibility and applicability to a wide range of practice settings and contexts, with ideas that can transfer to other teams facing similar or cross-cutting challenges.
Methods
Aligned with the multidisciplinary nature of cancer care, the educational program was multimodal and comprised of three main components: a collaborative learning exchange, an online module and an online resource hub. The collaborative learning exchange, “I-O ChangeMakers,” engaged a small cohort of learners (n=19) in a series of facilitated discussions around change management strategies and leadership development. The goal was for the participants to identify opportunities to improve clinical workflow processes and patient care at their institutions and design, implement and evaluate interventions to address them. With personalized guidance and support, the participants utilized the Active Implementation Frameworkᶦ and Plan-Do-Study-Act (PDSA) cyclesᶦᶦ to develop and lead action learning projects to address the problems and challenges they identified. The participants also provided feedback to the faculty via discussions and informal interviews, which helped enhance the curriculum and fostered continuous improvement.
To increase their foundational scientific knowledge, the participants were encouraged to complete the online module, I-O Biomarker Update and Testing Challenges. This interactive activity utilized case scenarios to increase knowledge around recent approvals of combination I-O therapies, emerging I-O biomarkers and challenges in biomarker testing. The online module also enabled the education to reach a wider audience beyond the cohort who participated in I-O ChangeMakers. The third component of the educational program was an Online Resource Hub: Improving I-O Delivery in Community Practice, containing a curated collection linking to related education. The hub also included a summary of project abstracts and videos from I-O ChangeMakers and ideas for QI projects that other multidisciplinary cancer care teams can undertake in their institutions.
Results
The program achieved a range of outcomes and impact, ranging from participation to improvements in knowledge, competence and patient healthᶦᶦᶦ Across the different educational activities, there were more than 1,600 participants from several healthcare roles and specialty areas, including pathologists, hematologists, oncologists, pathologists’ assistants, laboratory professionals, pathology trainees, physician assistants, nurses and other healthcare providers. Results of knowledge tests completed by the participants in the online module showed a statistically significant gain in overall knowledge of the testing, interpretation and implications of biomarkers, D = 27%, t(1586) = 41.3, p < 0.01, η2 = 0.5. Examples of knowledge gain in specific areas included knowledge of newly approved combinations of immunotherapies, the latest science on emerging biomarkers, and the consideration for the testing and interpretation of current and emerging biomarkers. Feedback from the participants implied how they planned to apply their learning, including changes they planned to make in their practice as a result of what they had learned. From the follow-up survey, there was evidence of follow-through as learners described changes they had made from 1 to 15 months after the education launched.
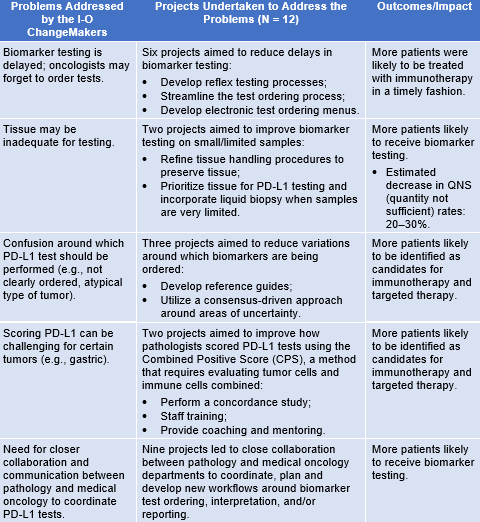
For the participants in I-O ChangeMakers, evidence of actual changes to practice was embedded into the QI projects that they designed and implemented. There were 12 improvement projects that addressed a wide range of systems-level challenges, as summarized in the table. The table also underscores how the participants, who were from varied types of practice settings, addressed cross-cutting problems and systems-level challenges to improve patient care.
Discussion
The results of the evaluation highlight how the approach was successful in achieving the program goals. In addition to increasing individual knowledge, skills and competence around I-O biomarkers and biomarker testing, I-O ChangeMakers enabled learners to apply what they learned to their individual practice and fostered team learning through peer-to-peer education, preparing learners to serve as effective change agents in their institutions. Thus, the educational program helped empower pathology teams to play a greater role in shaping and implementing institutional I-O policies/protocols to advance cancer care in their local communities, including addressing common factors in disparities in patient care. Furthermore, the evaluation highlights the clinical impact that the program had on patient care, with the QI projects enabling the participants to apply their learning, demonstrate leadership and facilitate change to make actual improvements in patient care.
Conclusion
As the landscape of I-O continues to rapidly evolve, there will likely be a continuing need for additional education and QI initiatives to ensure optimal biomarker testing and patient care. This project demonstrates how learners can be equipped and empowered to lead QI efforts. The diverse nature of the QI projects highlights the approach’s flexibility and applicability to a wide range of practice settings and contexts, and they provided a mechanism for identifying cross-cutting challenges to optimizing biomarker testing, patient care and successful approaches to overcoming them. This type of dissemination can be particularly beneficial for sharing ideas for QI projects that other multidisciplinary cancer care teams could undertake in their institutions. In addition, the online module and online resource hub maximized the reach of scientific knowledge for learners to apply in their practice.
Lessons learned from this project can be generalized and/or transferred to other teams facing similar challenges. They have also helped shape future education, as ASCP and Q Synthesis continue to build on this model through other cohort-based activities designed to empower learners to lead and make workplace changes to improve patient care.
Acknowledgments
This project was funded by an independent educational grant from Bristol Myers Squibb.
About the Authors
 Melissa Kelly, PhD, is senior manager in evaluation, measurement and assessment for the American Society for Clinical Pathology, where she oversees the evaluation of educational programs and related initiatives. In addition to expertise in evaluation, she also has experience working as an instructional designer and teaching courses in assessment and program evaluation.
Melissa Kelly, PhD, is senior manager in evaluation, measurement and assessment for the American Society for Clinical Pathology, where she oversees the evaluation of educational programs and related initiatives. In addition to expertise in evaluation, she also has experience working as an instructional designer and teaching courses in assessment and program evaluation.
 Joseph Kim, MD, MPH, MBA, FACEHP, CPHQ, is president of Q Synthesis LLC, an independent healthcare education and quality improvement company that advances interprofessional collaborative practice by applying principles of systems thinking, implementation science, and health services research. Some of his recent projects have focused on improving team-based processes around cancer biomarker testing, identifying and managing treatment-related adverse events, aligning treatment plans with clinical guidelines, and coordinating care in complex patient populations. Dr. Kim serves on the board of directors for the Alliance for Continuing Education in the Health Professions (ACEhp). He is also a past president of the National Association of Medical Education Companies (NAMEC). Dr. Kim holds a BS in engineering from Massachusetts Institute of Technology, an MD from University of Arkansas for Medical Sciences, an MPH from the University of Massachusetts Amherst, and an MBA from St. Joseph’s University.
Joseph Kim, MD, MPH, MBA, FACEHP, CPHQ, is president of Q Synthesis LLC, an independent healthcare education and quality improvement company that advances interprofessional collaborative practice by applying principles of systems thinking, implementation science, and health services research. Some of his recent projects have focused on improving team-based processes around cancer biomarker testing, identifying and managing treatment-related adverse events, aligning treatment plans with clinical guidelines, and coordinating care in complex patient populations. Dr. Kim serves on the board of directors for the Alliance for Continuing Education in the Health Professions (ACEhp). He is also a past president of the National Association of Medical Education Companies (NAMEC). Dr. Kim holds a BS in engineering from Massachusetts Institute of Technology, an MD from University of Arkansas for Medical Sciences, an MPH from the University of Massachusetts Amherst, and an MBA from St. Joseph’s University.
 Kellie Beumer is the director of learning innovations for the American Society for Clinical Pathology, where she oversees the instructional design and delivery of ASCP's live and online education and grant writing efforts. With nearly 20 years of experience, she is passionate about helping associations develop innovative medical education solutions aligned with best practices in adult education and learner needs. Her background is in molecular biology and instructional design, and she is currently working on her MBA.
Kellie Beumer is the director of learning innovations for the American Society for Clinical Pathology, where she oversees the instructional design and delivery of ASCP's live and online education and grant writing efforts. With nearly 20 years of experience, she is passionate about helping associations develop innovative medical education solutions aligned with best practices in adult education and learner needs. Her background is in molecular biology and instructional design, and she is currently working on her MBA.
ᶦ Fixsen DL, Naoom SF, Blase KA, Friedman RM, Wallace F. Implementation Research: A Synthesis of the Literature. University of South Florida; 2005.
ᶦᶦLangley GL, Moen R, Nolan KM, Nolan TW, Norman CL, Provost LP. The Improvement Guide: A Practical Approach to Enhancing Organizational Performance. 2nd ed. Jossey-Bass Publishers; 2009.
ᶦᶦᶦMoore DE Jr, Green JS, Gallis HA. Achieving desired results and improved outcomes: integrating planning and assessment throughout learning activities. J Contin Educ Health Prof. 2009;29(1):1-15. doi:10.1002/chp.20001